Hand in Hand at Home
 Practical, simple and effective tools that allow you to focus on what matters most – building a new approach to life with dementia. Feel empowered, rather than defeated. You can do this, and we will help you!
Practical, simple and effective tools that allow you to focus on what matters most – building a new approach to life with dementia. Feel empowered, rather than defeated. You can do this, and we will help you!
Moments We Relate To
What is a care partner?
If you are reading this, you are probably a care partner. Hand in Hand is founded on the premise that a person with dementia is part of our community and is not labeled by their illness. When talking about a person who cares for someone with dementia, the old term we used to use was caregiver. We like to say care partner instead because the person with dementia gives as much back to us as we give to them, this is why we are partners in this journey. When we speak about dementia care, to keep it clear, if we are talking about one person in the care partner dyad, we usually refer to the person without dementia as the “care partner” and the person with dementia as an “individual living with dementia.”
Individuals with dementia teach us how to listen, be patient, find joy in the small moments of life, love unconditionally, be flexible and how to be in the present.
Hand in Hand at Home
You have the power and the ability to change your perspective on dementia care, and we will walk you through it and show you how. We know dementia care can be challenging, but we’ll be with you every step of the way, helping you and your loved with dementia to live with more joy, dignity, community and independence. We have filled this website with hundreds of simple suggestions to help care partners just like you. We are sure you’ll find something that is the right fit for your situation. Browse through the topics at the bottom of the page and read about how to live the very best life with dementia.
Written by Jennifer Brush, MA, CCC/SLP
Making Each Day Easier
If you are care partner, stop for a minute, close your eyes and imagine you are a person who has been diagnosed with dementia. You wake up in the morning, the room is familiar, but you aren’t sure what you are supposed to do. Without changing out of your pajamas or washing up, you walk around the house looking for a clue about what might be going on. You find your spouse in the kitchen and sit at the table, hoping she will get you something to eat and wonder what is going to happen that day.
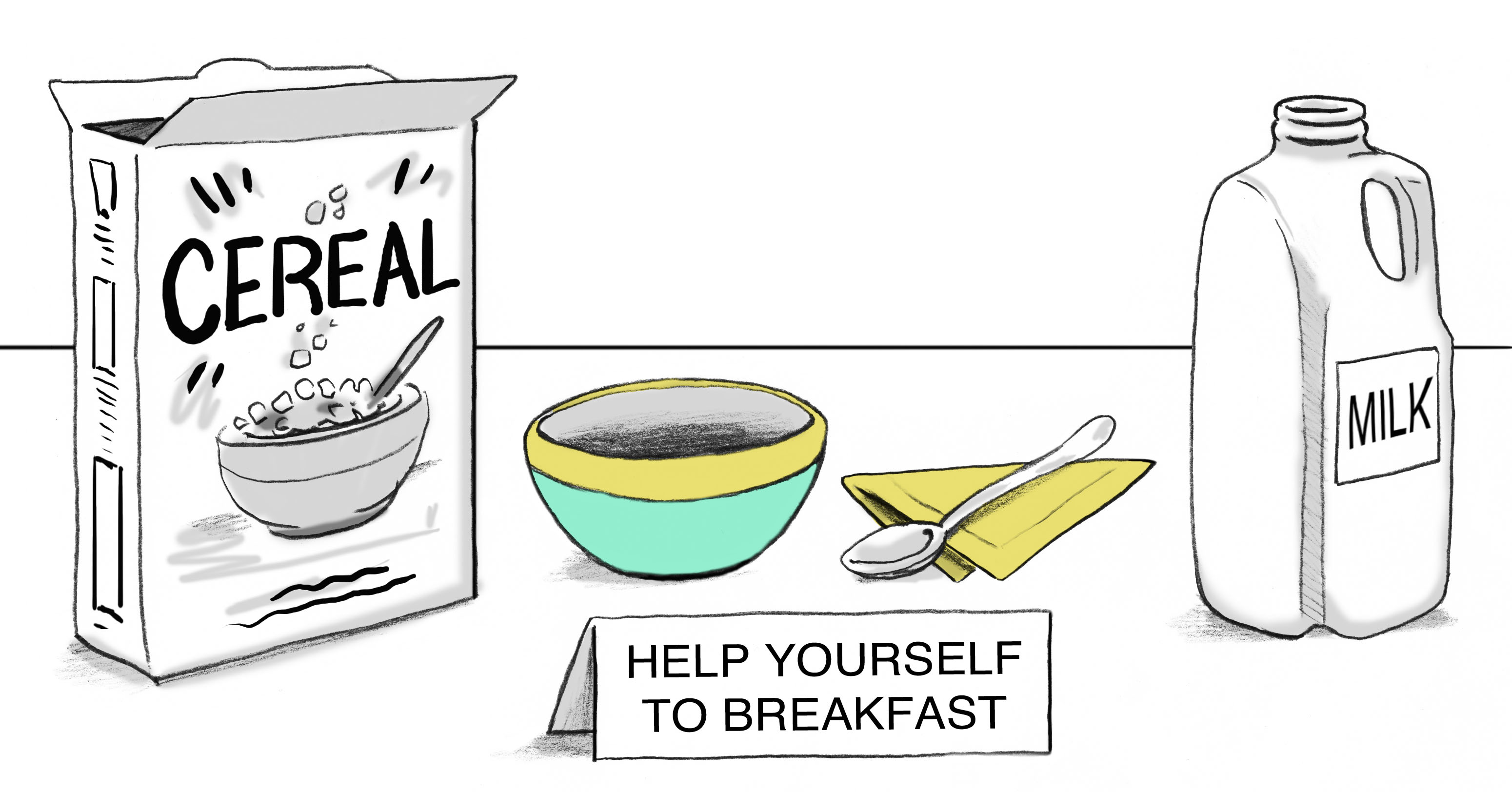 Or, imagine this situation. You are a person living with dementia. You wake up in the morning, the room is familiar, but there are clothes laid out for you in the order they should be put on. There is a friendly reminder to brush your teeth and head on for breakfast. You find your spouse in the kitchen. On the counter, there is a bowl, cereal and milk with a message for you that says, “Help yourself.” You make yourself breakfast and join your spouse. Together, over breakfast, you review the schedule of events for the day and write down the two chores you will do that morning.
Or, imagine this situation. You are a person living with dementia. You wake up in the morning, the room is familiar, but there are clothes laid out for you in the order they should be put on. There is a friendly reminder to brush your teeth and head on for breakfast. You find your spouse in the kitchen. On the counter, there is a bowl, cereal and milk with a message for you that says, “Help yourself.” You make yourself breakfast and join your spouse. Together, over breakfast, you review the schedule of events for the day and write down the two chores you will do that morning.
Which scenario would you prefer to experience?

“The purpose of our lives is to be happy.” Dalai Lama
In the past, dementia care has consisted of just keeping a person safe and contained, but this often leads to boredom, anxiety, increased confusion, depression and poor quality of life. We want to make sure that people with dementia are not only safe but that they have things in their life that they enjoy. We want them to feel loved and have a sense of control over their day. When we create a home environment that focuses on their abilities, wants and needs, we can decrease boredom, anxiety, confusion and the behavioral difficulties that come from those issues. Click here to learn more about unexpected behaviors and dementia. Does that sound appealing to you? We could all use more joy and less stress, right? But you are probably thinking, “I am too busy and too overwhelmed to do anything more than I am doing!” We understand. We have been in your shoes, we have all been care partners of someone with dementia too. This Coalition is made up of dementia care experts, who are researchers and clinicians and we have a trick or two up our sleeves to share with you. We would like to introduce you to something that will totally change the way you approach dementia care.
It’s called Hand in Hand at Home.
- We see the person, not the illness. Society often sees people with dementia as an illness and forgets to look at their abilities, needs and interests. We focus on the abilities that remain and work with those, rather than defining a person by abilities that they have lost. This means we create activities and daily roles in which the person can participate.
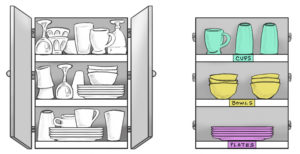
- We can help you to set the up home for success. When you look closely at the environment of a person with dementia, you can prepare that environment for success. For example, something as simple as taking the doors off the kitchen cabinets and labeling shelves can allow a person with dementia to take out and put away their own dishes again because they can easily see where the dishes go.
- We recognize individuals’ lives have meaning and purpose. Far too often, society treats people with dementia as if they have no meaning and purpose in life, but we do not believe that. We can help you to maintain a person’s roles and identity throughout the full course of their life with dementia. Identity and belonging are key factors in happiness and maintaining a good quality of life. No one wants to be treated as if they do not contribute to the world around them or like they have no independence.
- We demonstrate how to do things. We have found that it is helpful to set up tasks for people in a way that they can do them on their own as much as possible and then when they struggle, we guide them by showing them the step and inviting them to follow what we are doing.
- We believe behavior has a reason. When a person with dementia exhibits challenging behaviors, we do not assume the behavior is happening just because a person has dementia. We understand there is an unmet need that needs to be discovered and accommodated in order to help the person with dementia function well. For example, you could assume that a person with dementia who hits a care partner hits just because they have dementia. If we look closer though, we may see that the person is hitting because they do not understand why someone is taking their shirt off to help them get ready for bed. They may be hitting because they are scared or feel like no one cares.
- We use observation skills. Observation is essential to help another person be as independent and successful as possible. We always want to think of ourselves as observers. If we want to help a person take a bath more successfully, we need to first observe how bathing is currently going – what works, what doesn’t – and modify from there. Being observers also ensures that we focus on the person rather than assuming ability or behavior is due to dementia.
We are all familiar with the story of Goldilocks and the three bears. Whether it had to do to the feel of the bears’ beds or temperature of their porridge, Goldilocks was not pleased by the extremes. She wanted something that was “just right” for her. If we are going to truly partner with and support individuals with dementia, we don’t want their life to be too simple or too complex; we want it to be just right for them. That means, we have to spend a lot of time being observers and putting ourselves in their shoes. We have to learn how to step back and provide just the right amount of assistance – not too much, not too little. Too little assistance, then the persons struggles or is at risk of being injured, too much assistance and the person loses self esteem and independence. We also have to figure out what is the right amount of stimulation – not too much, not too little. Too much stimulation and someone may become agitated and anxious, too little and boredom and depression sets in.
Over time, because of the changes in the brain a person with dementia experiences, the type and level of stimulation and assistance a person requires changes. As the disease progresses, we have to make adjustments in the way we interact in order to support their need for independence, meaningful relationships and purpose – all critical for their well being.
So, how do provide the right amount of stimulation and assistance? We watch, we listen, we try, until we find what’s just right.
Here’s an example we’ve encountered. You’ve probably experienced something like it yourself.
Often when discussing dementia care, sadly, we are told about all of the things a person with dementia can no longer do. For example, it is often assumed that a person with dementia can no longer wash their hands because when some people with dementia go to the bathroom, they do not wash their hands. Maybe we remind them to wash their hands and they still don’t do it. Why might this be happening? People with dementia often become confused when there are many steps in a sequence. You and I may not think that there are very many steps in the sequence of washing your hands, but there are. If you make a list right now, you can probably come up with 10-20 steps for washing your hands!
Think about all of the common tasks we complete every single day. We shower, make our bed, get dressed, fix our meals, etc. Each one of these tasks has multiple steps. A person with dementia can experience a breakdown during any of these steps. When you notice someone having trouble with something you think is simple, pause a moment, be patient, try to figure out which step caused trouble or confusion. When we break an activity into its individual steps (task breakdown) and present one step at a time, people with cognitive impairment are more likely to achieve success.
We are here to help you find the feeling or place that is just right – for you and for your loved one.
There are simple strategies here on our site for everyone, we are sure you’ll find something that is the right fit for you. Browse through the topics below and find ones that interest you. There will certainly be many suggestions that jump right out at you because you are having some challenges. Read through the material and try some of the strategies that resonate with you. Make adjustments to fit your lifestyle and needs. But, make sure you try them! You’ll be amazed at how easily you can help your loved one go from stressed or confused to content or engaged. Use our Contact Us page to let us know what you tried and how it worked.
Hand in Hand at Home
There are simple things you can do to transform your home into a supportive place that helps your loved one with dementia function better. We are going to show you just how to do it.
What is Dementia?
Dementia isn't a specific disease. Instead, dementia describes a group of symptoms affecting memory, thinking and social abilities severely enough to interfere with daily functioning.
Transforming Your Home
The best home environment is one that supports the abilities of the people living there.
Declutter
Understand the negative impact of clutter and take steps to improve the home environment.
Enhance Lighting
Simple changes in lighting can be made in the home to help your loved one function more independently and sleep better.
Support Memory
Create a memory center in your home to reduce confusion and foster wellbeing.
Communicate Effectively
Use a style of communication that is easier for the person with dementia to understand and follow conversations.
Understand Behaviors
Make sense of unexpected behaviors and learn how to prevent them.
Walking About
Tips for understanding and preventing walking about as well as information about how to choose a locating device.
The Power of Choice
Given them every opportunity to make informed choices about their care, leisure time, clothing, food and anything else that affects their life.
Power of Purpose
We all need a reason to get out of bed each day. People with dementia need to know their life has meaning and purpose.
Hiring Home Care
Learn how to ease the transition to additional care partners find out what questions to ask.
Self-Care
Advice for taking care of yourself, learning how and where to ask for help and scheduling breaks from caregiving.
Get Started!
You can do this! Take one step at a time. Follow these steps to get started.